History of AMPATH Medical Record System (AMRS)
Video below shows both part 1 and part 2 of the lecture. Full text & slides below
Part 1: History of AMRS 00:00
- Problem of paper records 2:11
- Microsoft Access & OpenMRS System 8:48
- Building of AMRS POC 13:24
- The AMRS Team Today 17:31
- Demo of AMRS POC 20:58
- Upcoming Major Projects 30:33
Part 2: Current Data Capabilities & Future of AMRS [text and slides here]
- Current Clinical Data Capabilities 34:57
- New data visualization tools: Kibana 41:58
- Future of AMRS 50:52
Presented at AMPATH Partners Summit October 10, 2018 Eldoret, Kenya.
PART 1:
History of AMPATH Medical Record System (AMRS)
1. Introduction
I am interested in how we can design better healthcare systems, and in particular believe that technology & specifically electronic medical records play a crucial role in expanding access, improving quality, and reducing the cost of care.
Today, we will look at some of the dashboards at AMPATH and those that we are building to use data better.
But before we can discuss that, it is important to understand the evolution of the AMPATH medical record system, which collects and brings this data together.
As full disclosure - I have been here for not even 3 months. So, when I speak of the really cool things “we” have done - I did not have anything to do with it. It is really our talented Kenyan team. This photo is of our two major leads. On the left is Dr Jonathan Dick, an Internist from Indiana University and Professor at Regenstrief Institute. He is pictured with Nicky Kiborour our head developer.
2. Problem of Paper Medical Records
Let’s start at the beginning. At one time in AMPATH there was one patient. And obviously, its easy to keep track of just one patient.
We just need a folder, and some past medical history notes. Some notes from today’s clinic doctor visit, and the nursing notes, and nutritionist notes, and social worker’s notes. And nursing vitals, and physician exam. And the patient’s medication list, and past medication list, and their allergies.
And their recent viralload, and we also need copy of their past viral loads.
And a chest x-ray report. Wait. This shows they have tuberculosis. We also need to add more medications.
We’ll need to now track when they should come back. When they should repeat their labs. When they should repeat the chest X-Ray.
Oh, yes, and we sent them to a dermatologist to inspect a lesson for Kaposi sarcoma – so we’ll need to remember to await that referral, and follow up on the report when it comes back.
And when they become lost to follow up, we need a system to know that the very next day; so our retention worker can get on her motorcycle and drive to the client’s house to keep them in care.
OK. So that’s a lot of data to manage for just one patient, during one encounter.
Has anyone ever tried to manage their own personal medical record, or that of a family member? It's a surprisingly large undertaking.
Now try to imagine keeping track of a few hundred, or a 1000, or 5000 patient records as in this clinic. And imagine all the results to file, hundreds of charts to pull each clinic.
Some AMPATH record rooms held 5000 patient files per room.
Registers
And wait, we’re actually not done. Most of this information must be recorded in Ministry of Health registers for metrics purposes. So that means we need to copy the same patient information into 1, 2, 5, 6 or even more registers at once.
And its important to keep in mind that when reports from this data are created – the data is in aggregate (those few boxes at the bottom of the register are all that get passed on). If you wanted to get to the raw data it is still sitting in paper registers off somewhere in a warehouse.
This is what the electronic medical record has displaced.
How can you really know the quality of care each of these patients received if you can’t see that data, in real time, and allow it to help drive care?
Without data from the system we don’t know if we are spending each dollar effectively.
I was in a clinic yesterday with Dr Laktabai, and he noticed that the clinic there has found a use for paper medical records.
The story ofAMRS has been one of continuously working to improve our data and in order to provide better care to patients.
3. Microsoft Access & OpenMRS System
From the start, AMPATH realized the value of an electronic medical database as a crucial component in HIV care.
Very early on a Microsoft Access Database was used. Paper records were entered into the database, and it would provide reports.
But by2004 AMPATH had around 3000 patients, and it was anticipated over the next 1-2 years they would grow to 30,000patients. And so, the Access Database was stretched beyond its limits. It had reached the maximum number of columns in the Access tables, and on the second and third data tables.
AMPATH brought informatics expertsfrom the Regenstrief Institute in Indiana to study the problem.
The Regenstrief Institute was founded by the Dishwasher King – Mr Sam Regenstrief – who was an expert in system efficiency and founded the institute to study how to apply systems design and informatics to healthcare.
When Paul Biondich and Burke Mamlin arrived in Eldoert, it was immediately apparent to them the enormous scale of an informatics system required to battle HIV.
Therefore AMPATH looked for other groups to join in. Partners in Health (Dr Hamish Fraserand Darius Jazayeri) who were facing similar challenges of growing their HIV IT system as they moved rural Haiti into Rwanda. Additional early partners were the South African Medical Research Council (Chris Seebregts), and the Millennium Villages Project (Andrew S Kanter).
Java was selected as the language for the system as Partners in Health had build their previous system in Java. A MySQL for database is used.
The system was also built upon ‘concept dictionaries’ where information is stored using libraries of terms, so that each term can be retrieved. This underlying architecture was significantly influenced by Regenstrief’s extensive expertise in this area and their work with Loinc. The data structure was designed to work for any condition, and this is a current data model.
This global team worked for two years, and in February 2006 the first instance of the OpenMRS system was launched in Eldoret. The version of OpenMRS running at AMPATH was called the AMPATH Medical Record System - AMRS
In the coming years the global community would grow to thousands of collaborators, the support of Google Summer of Code for over a decade, and today OpenMRS is used in over 80 countries.
The first system
In the first system, paper forms were filled out in clinic, and then transported to a data entry facility to be entered retrospectively. The forms were then re-transported back to the clinic to be refiled.
The system would also produce a patient data summary. It had past history, lab summaries, and even clinical decision support reminders.
But there was significant difficulty getting this single sheet filed into the charts in a timely manner. This meant the summary sheets were often out of date, and unreliable.
The system was also running off of microwave satilite dishes pointed at each other, which was expensive and often broke and hard to maintain.
4. Building AMRS Point of Care (POC)
A decade later, by 2015 technology had undergone massive changes.
Tablets had been invented and were affordable.
Cellphones and mobile were commonplace, and Kenya was ahead of the world.
The idea of building a real time point-of-care system was feasible.
But there were implementation challenges in be solved.
There was not a reliable power supply in many facilities. Therefore solar panels and a battery backup were installed to provide sufficient power.
3G and later 4G Safaricom cellular was installed.
This was connected to a router system to connect this to the tablets.
This is connected via a dedicated encrypted line direct from the clinic through Safaricom, into our central server. The data center is a climate controlled, biometric protected space with significant battery backup, and a powerful central server that runs the entire network.
The first pilot of the point of care system was tried October 2015. The pilot went horribly. People hated it. But within four months AMRS had tweaked the system, and the first sucessufl pilot in Burnt Forest took place (Feb 2016). And then, the team got to work.
Two years later, today, the system is used six days a week, and there are 500+ unique users
It operates live as a point of care system at 25 high volume sites serving 61,000 patients, and is used as a retrospective data entry system at the remaining 34 low volume sites (planned to be converted to POC).
To date, almost 8 million visits have been recorded. And around 250 million discrete questions asked of patients in our database.
I’ll be the first to admit the system is not perfect, and we acknowledge there is much work to be done. But step by step the system continues to improve.
5. The AMRS Team Today
Lets look at how AMRS operates. This is a picture of many on our team last Friday at the Sprint Demo. Our team continues to grow and it looks like we may need different venue.
The team works the same as tech startups in Silicon Valley. We use Agile workflow – and work in two week “Sprints”. At the end of a Sprint, the whole team meets on Friday morning at a Sprint Demo where everyone shows their work.
It starts with the Project Manger– who is assigned to a department (such as HIV, or CDM, or Oncology) to meet with those users and their leadership to understand their needs, develop new projects.
Then our team of developers get to work on the code. We have amazing senior developers, interns (of which five just joined last week), and attaches’ who are university students under mentorship from the senior developer.
If you know any senior developers in Eldoret, please let us know.
We have a separate team, the Forms and Concepts team, that builds the forms which drive the clinical encounters.
Before software can be released, it must be thoroughly tested by Quality Assurance Team to find bugs.
Then the Implementation Team develops release notes and communicates updates to our users. The Implementation Team is also a powerful education squad who goes into new sites to educate and set them up on POC.
Users who have questions or trouble with the system contact our HelpDesk via telephone or text message. Any user can also submit Feedback via the app that comes directly through Slack to our Project Manager team.
None of this would be possible without the Network and IT team, that installs and monitor the routers, cellular connections, server, and hardware.
The system ultimately takes care of patients and produces a lot of data – this is coordinate by our Data and Analytics Team that work with AMPATH and ministry M&E (management and evaluation) to produce the necessary reports for the government and donors.
This may sound like quite a large team, but if you have ever funded health IT projects in the past – you know that health IT funding is a blackhole. It is remarkable how much has been accomplished by this team in such a short period, and with such minimal funding – compared to what is typically required to deliver an electronic medical record.
I’m incredibly proud of the AMPATH IT team. They really are the heart that makes the system work. They are dedicated, and continue to improve themselves by concurrently taking night courses in project management and informatics.
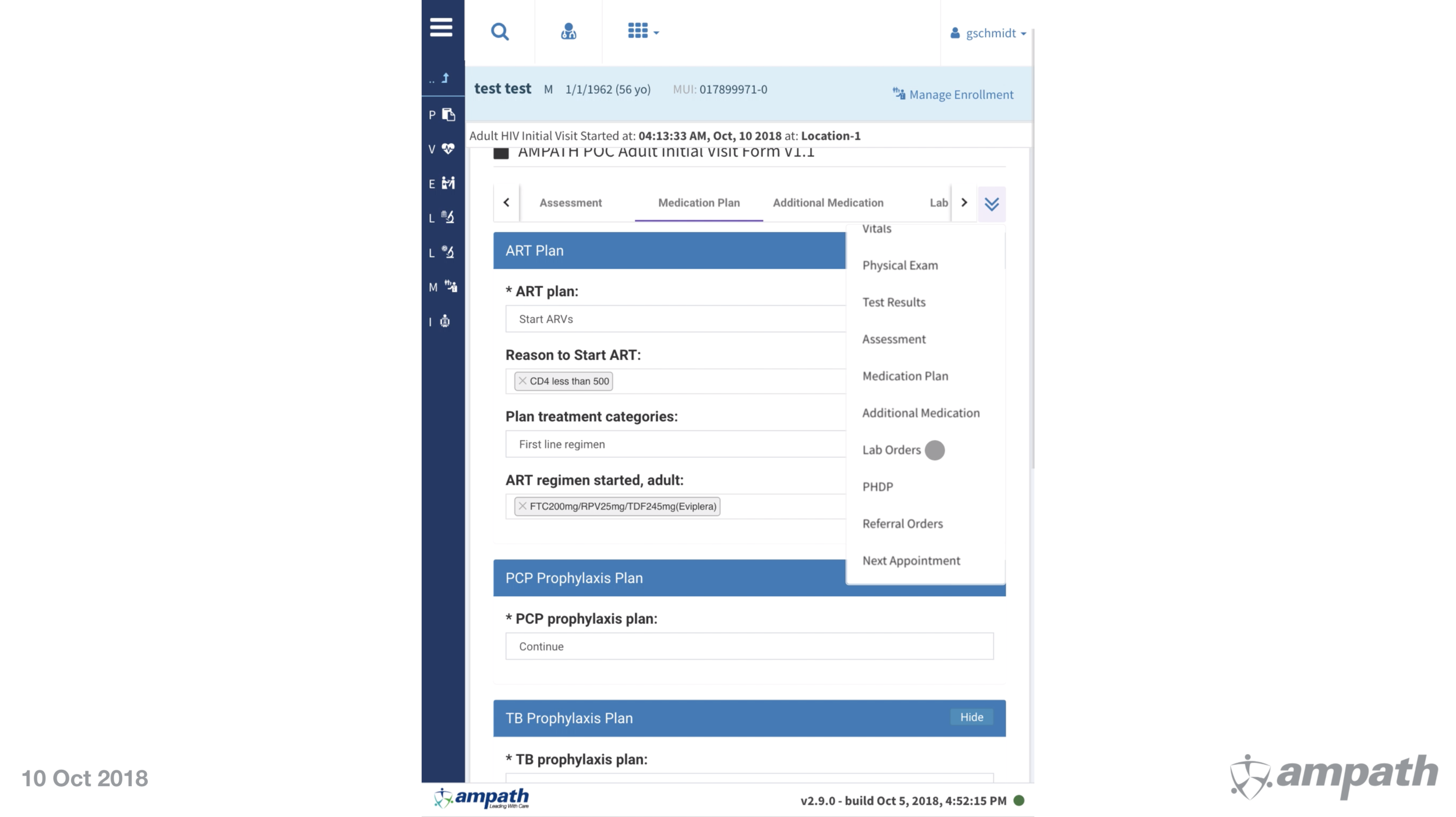
6. Demo of AMRS POC
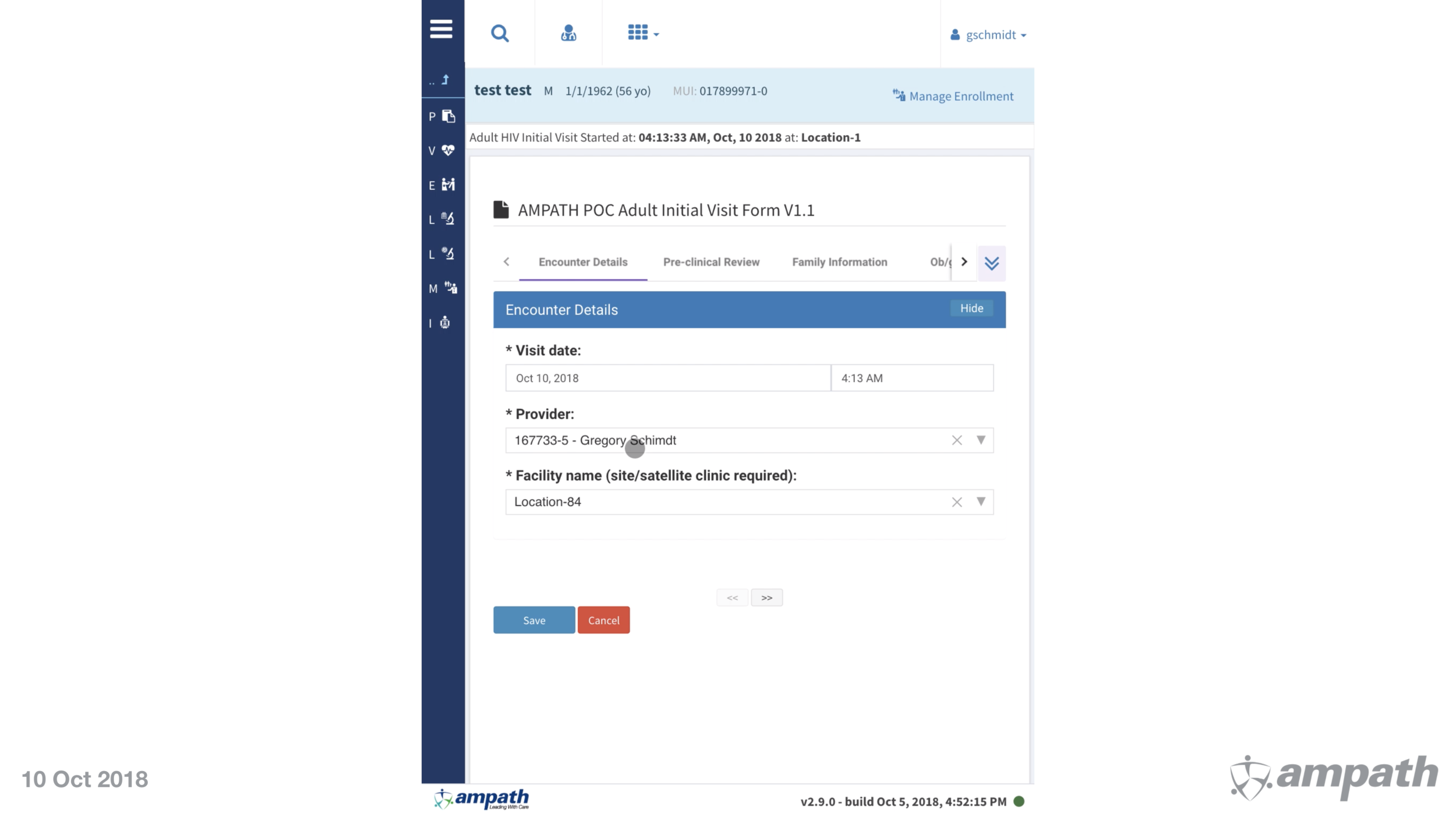
Let's boot up the system. It works on tablet or desktop.
This is the login screen. We can search for a patient by the AMPATH number or name.
Patient search
Patient demographic data.
Program summary page
There are helpful Clinical Decision Support Reminders that monitor a patient’s chart and suggest to Clinicians tests to order, programs the patient qualifies for.
HIV Summaries
Visits
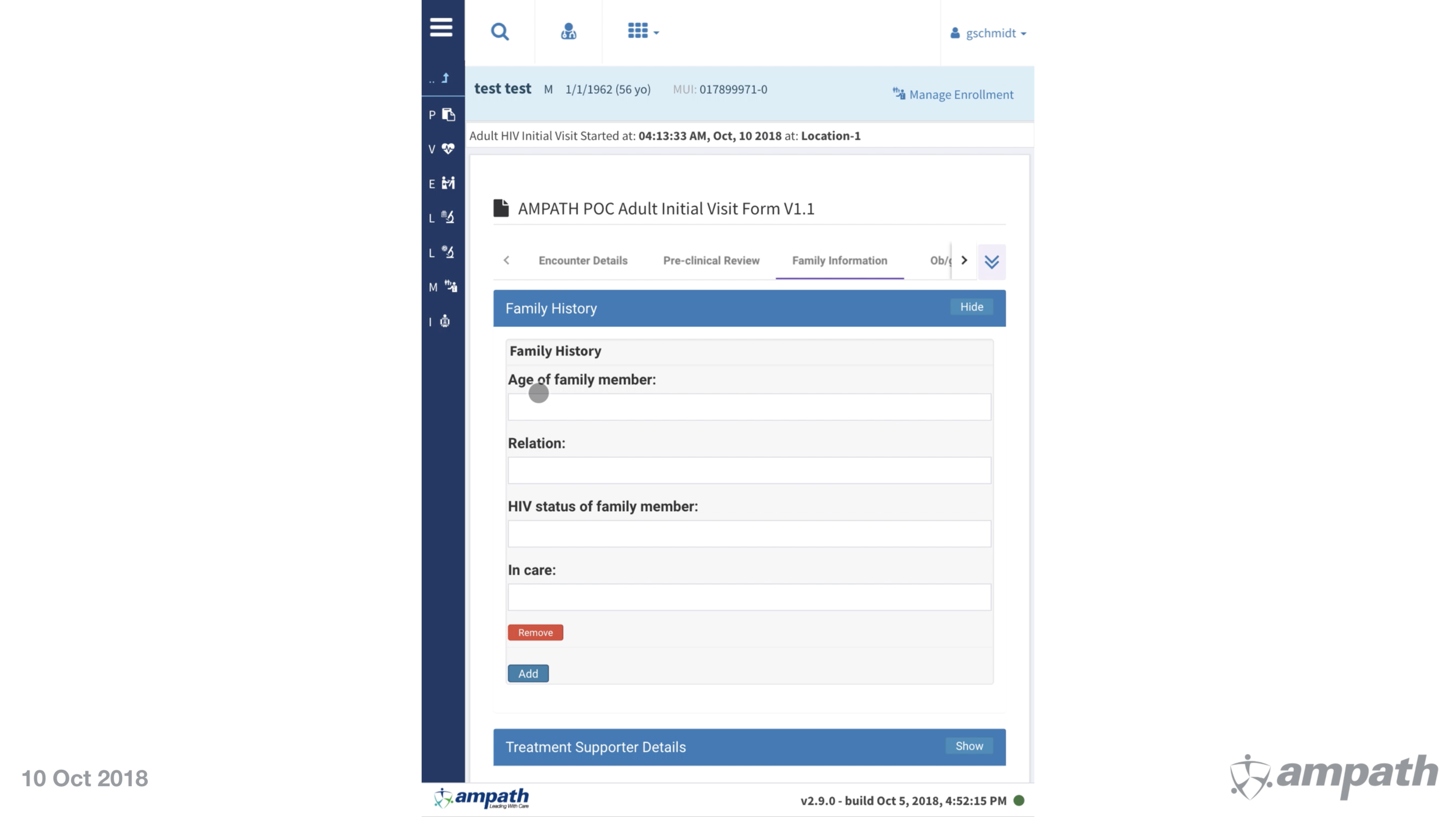
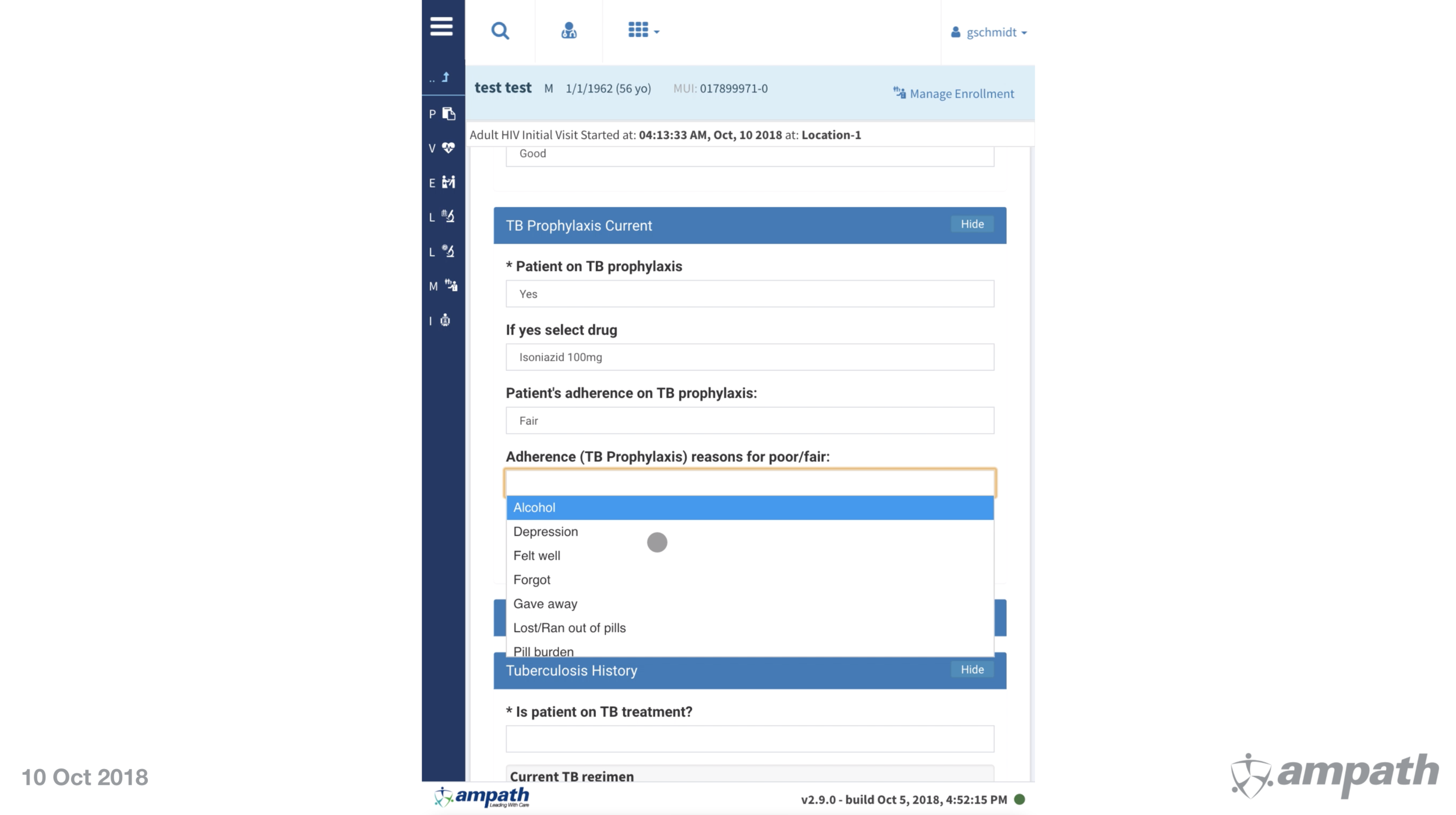
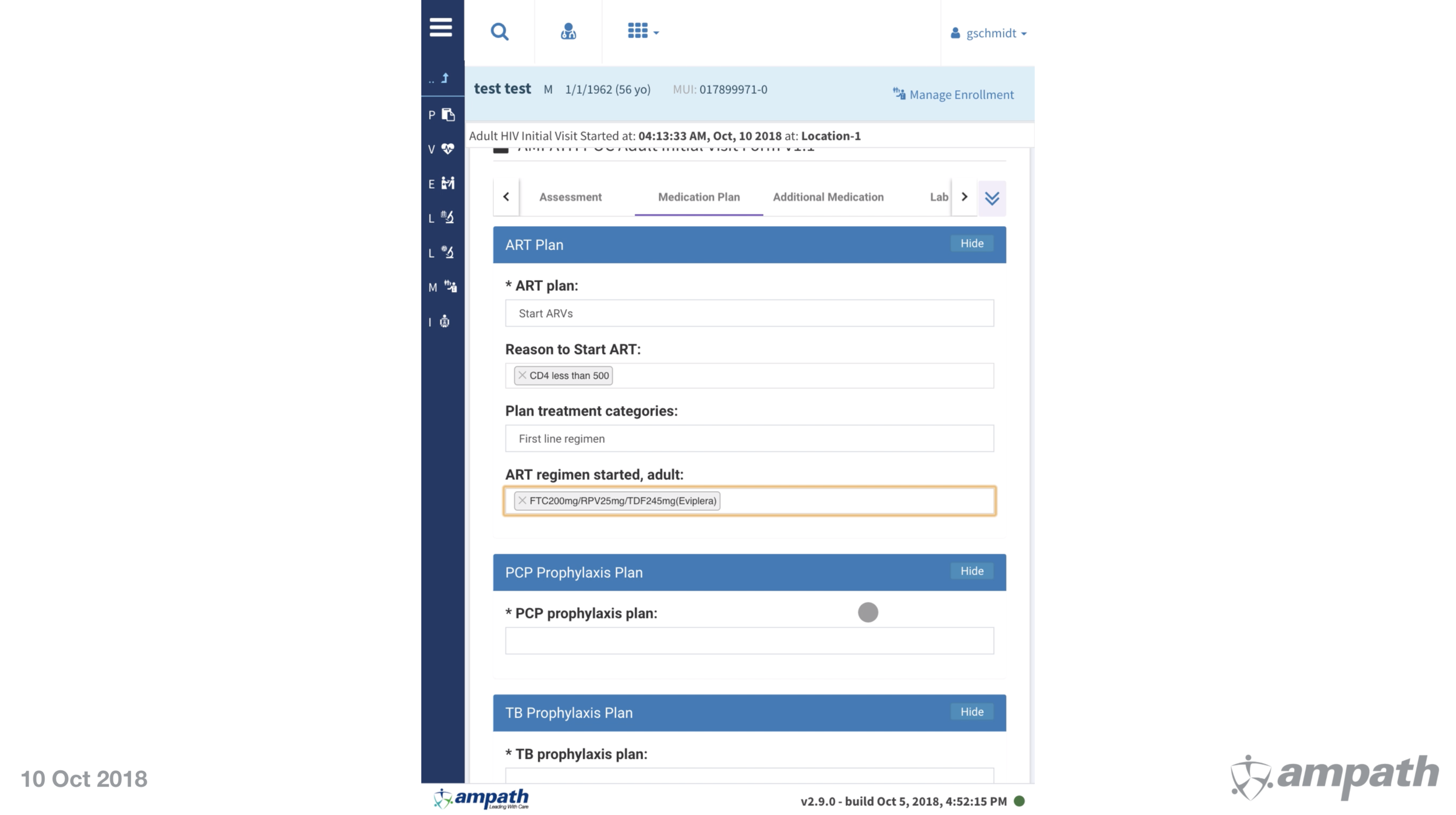
Example HIV New Visit Form. The form has lots of skip question logic and validation questions.
Beyond the EHR have other integrations. The HIV main lab prints labels for blood samples. The HIV lab data is then pulled in real time into the HIV Lab.
AMPATH in conjunction with the county developed a mobile XR Truck. In fact, they have now have two. This goes between the clinic network screening for Tuberculosis and pneumoniae.
It is fully equipped to operate in the field, with generator, its own air circulation system given the risk of TB patients, shielded truck walls.
Inside the patient has their image taken. It appears on this laptop. A copy is burnt to a disk, and the original sent wirelessly to our database.
The truck has other point of care diagnostics, and we look forward to adding more.
A few weeks ago we integrated these images directly into POC. And look at how fast they pull up in our software. This PACs system was built for HIV, but we can use the foundational infrastructure to store copies of scanned reports and pathology for Oncology.
7. Upcoming Major Projects
Additional clinical functionality
When AMRS designs new modules, it is always consider how one module can benefit not just the group that needs it but the entire POC system.
For instance, in the past few months for Population Health a referal tool was designed to seamlessly refer a patient up or down a level of care. This system will now also benefit Cardiology, and HIV.
Another example includes the patient feedback application that was demoed last Friday. It allows patients at the end of an appointment to anonymously submit feedback. This was built originally for chronic disease management programs, but when we met the QA lead from HIV program in line at the cafeteria we discovered they could use the same tool for new forms they were developing.
Looking to the near future a few specific areas we are looking at include
- Full order entry of medications and integration into the pharmacy
- Telehealth capabilities, to help keep patients close to home
- Integrate more diagnostic tools and labs
More Point of Care Sites
Over the coming quarters we will continue to expand the use of the AMRS point of care system. There are discussions to convert the sites that retrospectively enter paper clinical forms into AMRS to full point of care system; to extend it through the maternal child health; to add more oncology, chronic disease management population health, cardiology, dermatology, mental health, acute care, neurology.
We estimate that there are at least 100 new clinical sites on the horizon. This is a 5 fold increase in the number of current POC sites. And does not include the potential expanded territory of AMAPTH.
Further improve system speed and stability
A top priority is continuing to improve the stability and speed of the system, in particular in low connectivity settings. Uptime last year exceeded 95%, but this is not good enough.
More user training & support
We are introducing short screenshot training videos before the upgrade to new releases as well as creating an online AMRS University with video content. This will supplement the already extensive in person training, phone and text message support, and written help documents.
This concludes Part 1
Move onto: Part 2: Current Data Capabilities & Future of AMRS

